📌 Lesson Overview
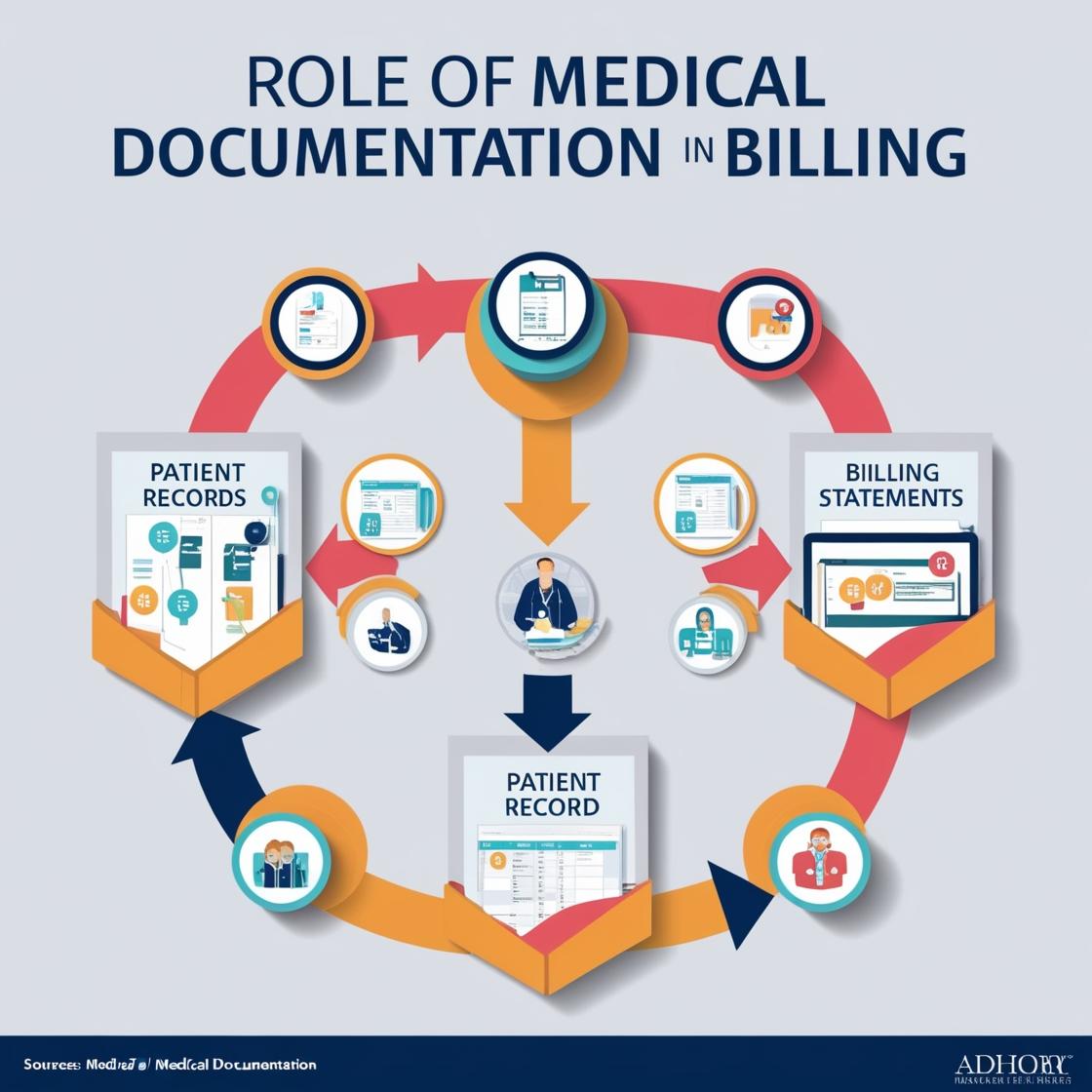
Accurate medical documentation is the cornerstone of effective billing. This lesson explores how detailed patient records directly impact the billing process, covering key components of documentation, the consequences of errors, and the crucial link between documentation and coding.
- Key Components of Medical Documentation for Billing
Medical documentation serves as the foundation for accurate billing, ensuring that services rendered are properly recorded and justified.
- A. Essential Documentation Elements
- Patient Demographics and Insurance Information:
- Ensures accurate patient identification and billing.
- Example: Incorrect DOB leads to claim denial.
- Chief Complaint (CC) and History of Present Illness (HPI):
- Provides the reason for the patient’s visit and supports medical necessity.
- Example: “Patient presents with acute onset of chest pain.”
- Physical Examination (PE) Findings:
- Documents objective findings and supports diagnosis.
- Example: “Lung sounds clear bilaterally.”
- Diagnosis and Assessment:
- Specifies the patient’s condition and justifies treatment.
- Example: “Diagnosis: Acute bronchitis.”
- Treatment Plan and Procedures Performed:
- Records the services provided and supports coding.
- Example: “Prescribed albuterol inhaler.”
- Medications and Allergies:
- Vital for patient safety and can impact coding.
- Example: “Allergy to penicillin.”
- Time Stamps and Signatures:
- Establishes the timeline of events and verifies documentation.
- Example: “10:00 AM, Dr. Smith.”
- Patient Demographics and Insurance Information:
- 📌 Example Breakdown:
- Detailed HPI: “Patient reports experiencing severe abdominal pain for the past 24 hours, radiating to the back. Pain is described as sharp and constant, worsened by eating. Patient also reports nausea and vomiting.”
- This level of detail supports a more specific diagnosis and coding.
- Detailed HPI: “Patient reports experiencing severe abdominal pain for the past 24 hours, radiating to the back. Pain is described as sharp and constant, worsened by eating. Patient also reports nausea and vomiting.”
- Impact of Inaccurate Documentation on Billing
Errors in medical documentation can lead to significant billing issues and compliance risks.
- A. Common Documentation Errors and Consequences
- Incomplete Documentation:
- Leads to claim denials and delays.
- Example: Missing diagnosis code.
- Inaccurate or Conflicting Information:
- Raises red flags during audits and can lead to penalties.
- Example: Contradictory information between the HPI and PE.
- Lack of Medical Necessity Documentation:
- Results in denials for services deemed unnecessary.
- Example: Ordering expensive testing without proper reasoning documented.
- Failure to Link Diagnosis to Procedure Codes:
- Claims are denied due to lack of medical necessity.
- Example: Procedure code for a knee injection without a corresponding diagnosis of knee pain.
- Incomplete Documentation:
- 📌 Example Usage:
- EHR Note: “Pt seen. Follow up.”
- Translation: This note is insufficient for billing, lacking details about the patient’s condition and services provided.
- EHR Note: “Pt seen. Follow up.”
- Case Studies: Linking Documentation to Coding
Analyzing real-world scenarios demonstrates the direct correlation between medical documentation and accurate billing.
- 📌 Case Study:
- A 70-year-old female presents with shortness of breath, cough, and fever. The physician documents a diagnosis of pneumonia and orders a chest X-ray and antibiotics.
- Coding Breakdown:
- ICD-10 Code for Pneumonia: J18.9
- CPT Code for Chest X-ray: 71045
- CPT Code for office visit: 99213/99214 depending on level of service.
- HCPCS Code for antibiotic administration.
- 📌 Key Takeaway:
- Detailed and accurate documentation enables coders to select the appropriate codes, ensuring proper reimbursement and compliance.
🔎 Key Takeaways
- ✅ Medical documentation provides the basis for accurate billing.
- ✅ Incomplete or inaccurate documentation leads to billing errors and compliance risks.
- ✅ Case studies illustrate the practical application of documentation in coding.
- ✅ Proper documentation supports medical necessity.